How is patient experience feedback used to improve the quality of adult inpatient mental health care in NHS England?
EURIPIDES is the short title for Evaluating the Use of Patient Experience Data to Improve the Quality of Inpatient Mental Health Care study. EURIPIDES aimed to understand which of the many different approaches to collecting and using patient experience data are the most useful for supporting improvements in inpatient mental health care.
Researchers from the EURIPIDES study team have made a series of recommendations for improving the way that NHS mental health trusts collect and use patient feedback to improve the quality of care for mental health inpatients. In this post, Dr Sarah-Jane Fenton summarises some of the key findings ahead of the full report being published in early 2020 as health research academics call for NHS to act on mental health patient feedback.
What was the study about?
The project examined how patient experience and feedback is managed in inpatient mental health care settings. To ensure the patient voice is heard, NHS Trusts are required to collect feedback from patients routinely. We do not know what kinds of feedback are most important or what management processes are needed to translate this into effective action plans, and we do not know if this makes any difference to patients themselves.
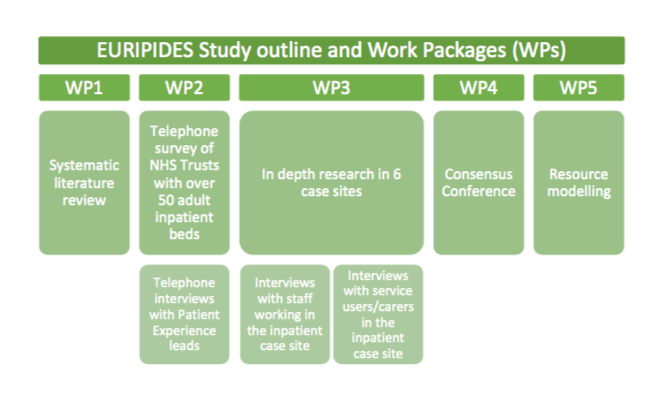
In order to explore this area, the proposed research had 5 work packages that are linked to the 5 study aims:
After completing a systematic review to identify patient experience themes relevant to mental health care (Aim 1), we will identify, describe and classify approaches to collecting and using patient experience data to improve inpatient mental health services across England (Aim 2).
We will use this information to choose 6 Trusts around the country for in-depth case studies where we will carry out interviews to find out what works for whom, and where (Aim 3). We will look particularly for evidence of meaningful service user and carer involvement, and for service improvement activity. We will present our findings to experts (including service users and carers) at a ‘consensus conference’ to agree on recommendations about best practice (Aim 4). We will ensure that our results are anchored in what is acceptable, feasible and sustainable in real-world NHS settings.
Finally, we will use health economics to predict the costs that would arise (and savings that might occur) if ‘best practice’ in collecting and using patient experience data was widely adopted, and we will speak to senior NHS colleagues to explore obstacles to adopting best practice (Aim 5).
The Work Packages are shown in a diagram above to show how the research activities fit together.
This was a collaborative study funded by National Institute for Health Research (NIHR), with a team from the Universities of Birmingham, Warwick, Sheffield and Queen Marys London, together with the Mental Health Foundation.
What are the key findings from the research?
From interviews conducted with staff and patients across NHS mental health trusts in England and found that few are collecting patient feedback to actively improve services. Of those trusts that do, only a quarter put their feedback to good use but, still only used it to create environmental rather than change to care services. We found that service improvements should never be led by complaints alone; but by listening to what works well for patients, NHS trusts have a real opportunity to empower both staff and patients.
Dr Sarah-Jane Fenton, a researcher in the School of Social Policy at the University of Birmingham, said:
“All NHS Mental Health Trusts are required to collect patient feedback, but prior to this study, we did not have an understanding of how they were using this information. This is the first study to look at how patient experience feedback is used in inpatient mental health settings to drive change and improve the quality of services.”
A key finding that could change the way NHS mental health trusts collect patient experience data was that patients staying on mental health wards are never too ill to give feedback, but prefer to do so towards the end of a hospital stay to clinicians they know and trust.
Even so, it was found that it was also important that those clinicians not only provided the opportunity for an on-going dialogue about a patient’s care during their stay, but for their relatives, carers or guardians to be able to feedback without the fear of negative repercussions for the patient. Dr Fenton said:
“The key message from this study is that no one is too unwell to tell you how they are experiencing their daily care - this combats some of the myths that persist resulting in people not seeking feedback from inpatients in mental health services in order to inform quality improvement work.”
This video (above) summarises the key findings across the study. In addition, we have produced a policy briefing, which is available here.
The briefing has been published ahead of the full study report, which makes 18 key practice recommendations for how NHS mental health trusts collect and use patient feedback.
Why does this research matter? How will it make a difference?
Every Trust collects patient feedback data, and in some cases they have spent years setting up local systems for this. We aimed to learn what works best from the wide range of current approaches. Our results provide the first comprehensive overview of current approaches to collecting and using patient experience data to improve inpatient mental health care in England. Dr Fenton suggests:
“For clinicians, this report is useful as it highlights the need to learn from positive feedback as well as negative. It emphasises the importance of staff being supported to have the time, support, and skills in order to build trusting relationships with patients that enables them to listen and respond to feedback.”
The research, and our recommendations, are grounded in the real world NHS. We have reviewed the study findings and agreed recommendations based on what is judged feasible, acceptable and sustainable according to commissioners, service providers and service users and carers. We hope that this research will inform the future collection, management and use of mental health inpatient experience data and thereby improve services. Professor of Mental Health and chief investigator of the study, Scott Weich, from ScHARR’s Mental Health Research Unit, said:
“Our policy briefing published today highlights the key findings and our guidance for NHS mental health trusts in how they can make best use of their valuable patient experience data. We have engaged NHS stakeholders at every step of the study to ensure our findings were practicable, so today we are calling on organisations like NHS England, the Department of Health and Care Quality Commission to support the NHS providers to implement the upcoming recommendations and drive service improvements centred around patient needs. There will be resource implications of adopting effective models to drive service improvements, but when used alongside patient outcomes and safety data to drive change, this leads to fewer patient safety incidents, better outcomes for patients and staff feeling more empowered to improve services.”
Find out more
This study is now complete. Our final report is due to be published in 2020 and can be found in the National Institute of Health Research Library. You can register with the library to be notified automatically when it is released. To give feedback to NHS Trusts in a timely manner, we have also produced a policy briefing being hosted by the University of Birmingham and the University of Sheffield. A summary of our key findings can be found in this video.
Funding
This research was funded by the National Institute for Health Research’s Health Services and Delivery Research (NIHR HS&DR) Programme.
About the University of Birmingham and the Institute for Mental Health
The University of Birmingham is ranked amongst the world’s top 100 institutions. Its work brings people from across the world to Birmingham, including researchers, teachers and more than 6,500 international students from over 150 countries. Through interdisciplinary research the Institute for Mental Health works to improve the outcomes and care for young people with mental health problems. We will do this by working together to understand the causes of poor mental health, prevent mental health problems from developing, and respond to established illness by developing new treatments and services.
About the National Institute for Health Research (NIHR)
The National Institute for Health Research (NIHR) is the nation's largest funder of health and care research. The NIHR:
Funds, supports and delivers high quality research that benefits the NHS, public health and social care
Engages and involves patients, carers and the public in order to improve the reach, quality and impact of research
Attracts, trains and supports the best researchers to tackle the complex health and care challenges of the future
Invests in world-class infrastructure and a skilled delivery workforce to translate discoveries into improved treatments and services
Partners with other public funders, charities and industry to maximise the value of research to patients and the economy
The NIHR was established in 2006 to improve the health and wealth of the nation through research and is funded by the Department of Health and Social Care. In addition to its national role, the NIHR commissions applied health research to benefit the poorest people in low- and middle-income countries, using Official Development Assistance funding.
This work uses data provided by patients and collected by the NHS as part of their care and support and would not have been possible without access to this data. The NIHR recognises and values the role of patient data, securely accessed and stored, both in underpinning and leading to improvements in research and care: www.nihr.ac.uk/patientdata.